Key details
-
Current treatment limitations: While ischaemic strokes – which account for nearly 90% of all strokes – are currently treated with clot removal and supportive rehabilitation, there remains a significant unmet need for therapies that directly address neurological consequences.
-
Stem cell potential: Mesenchymal stem cells (MSCs), particularly those from the umbilical cord (UC-MSCs), are a key focus in regenerative medicine due to their ability to regulate the immune system, reduce inflammation, and aid tissue regeneration.
-
Treatment development: A recent Phase 2 randomized controlled trial demonstrated that UC-MSC treatment is safe, with patients showing improvements in neurological deficits, quality of life, and functional independence compared to a control group receiving only rehabilitation.
-
Administration route: The trial compared intravenous (IV) and intrathecal (IT) (spinal canal injection) delivery methods, finding that the IV group experienced fewer procedure-related adverse events and demonstrated statistically significant improvements in functional independence earlier (at 6 months) than the IT group.
What is an ischaemic stroke?
An ischaemic stroke occurs when a clot cuts off blood flow to a part of the brain, preventing brain tissue from receiving oxygen and nutrients. This is a medical emergency, as strokes can happen suddenly and brain cells begin to die within minutes from a blockage happening.[1]
Stroke is a leading cause of death and disability worldwide[2], with ischaemic strokes being the most common, accounting for just under 90% of all strokes.[1]
The consequences of stroke can be severe, and may include:
-
Paralysis
-
Sensory changes
-
Speech or language problems
-
Vision problems
-
Cognitive impairments and memory loss
-
Emotional and behavioural changes.[3]
What treatment is available for stroke and its consequences?
Immediate treatment for ischaemic stroke, provided the patient arrives at the hospital in time, can include:
-
Thrombolysis: using a clot-dissolving medication to break up clots in the brain.
-
Thrombectomy: surgical removal of the clot using a clot retrieval device.[4][5]
This is followed by treatment to reduce the risk of another stroke, such as blood-thinning medication and, potentially, surgery to remedy narrowed arteries.[5]
Treatment for stroke complications is primarily supportive, and focuses on rehabilitation and recovery. Because each stroke is unique, this can vary widely, as it will focus on relearning lost skills and enabling as independent a life as possible. It can involve physiotherapy, speech and language therapy and occupational therapy.[6][7][8]
In other words, recovery and rehabilitation treatment focuses on helping stroke patients adapt to their “new normal”, whatever that may be, leaving a significant unmet need for a treatment that could directly address the neurological consequences of a stroke.
How could stem cells help with the consequences of stroke?
Mesenchymal stem cells (MSCs) are powerful cells which can be obtained from various sources, including bone marrow, adipose (fat) tissue, the umbilical cord and the placenta. These cells have the ability to self-renew and turn into other cell types, such as bone, fat, and cartilage; they can help regulate the body’s immune system and reduce inflammation, promote the formation of new blood vessels, and can release molecules and growth factors which aid in tissue regeneration.[9]
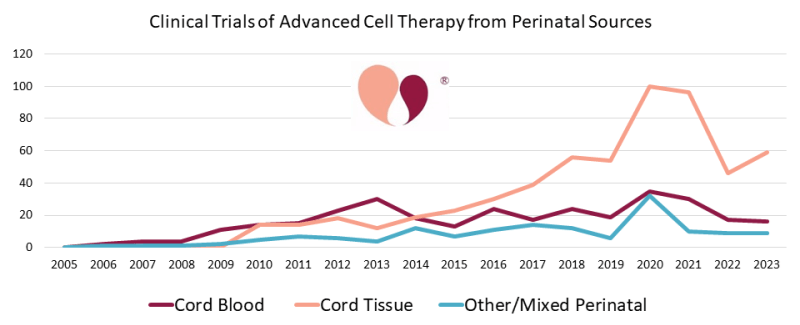
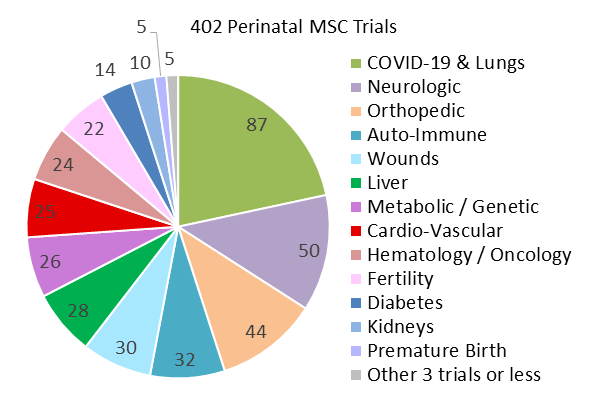
These properties have made them a key focus of the regenerative medicine field, with numerous studies and clinical trials investigating their potential as a treatment for many illnesses and conditions which currently lack effective treatments or cures. MSCs derived from the umbilical cord (UC-MSCs), in particular, have shown in preclinical and clinical studies that they could serve as a safe and potentially effective treatment for the neurological deficits associated with ischemic stroke.[10]
In order to develop a treatment, researchers need to not only identify the best source of stem cells, but also the most appropriate dosage as well as the most effective administration method. It is in this context that a recent clinical trial comparing two different methods of administration places itself.
What were the structure and findings of the clinical trial?
The phase 2 randomised controlled trial evaluated the safety and efficacy of UC-MSCs delivered either via IV (into a vein) or intrathecally (into the spinal canal) for treating neurological deficits after ischemic stroke.
The study involved 32 patients aged 40–75 years who were in the subacute or chronic phase of stroke recovery (7 days to 24 months post-stroke):
-
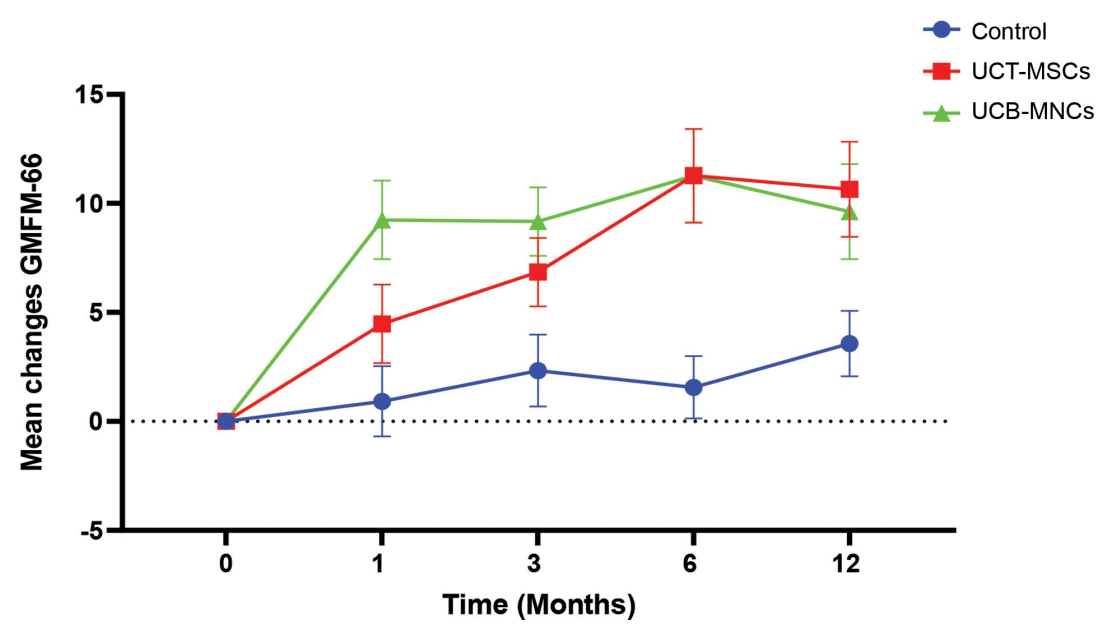
Patient groups: Patients were randomly assigned to receive UC-MSCs via IV or intrathecally (IT), in addition to standard rehabilitation therapy. A control group consisting of 16 more patients was created by matching patients one-to-one with those in the intrathecal group based on gender, age, and severity of stroke consequences as determined using the NIH stroke scale (NIHSS). This control group only received rehabilitation therapy.
-
Dosage: Patients in the treatment group received a dose of 1.5 × 106 cells per kg of body weight at baseline, and then again 3 months after the first dose.
-
Rehabilitation: Standard rehabilitation therapy consisted of 30 sessions designed to improve cognitive ability, motor function, and overall quality of life, each lasting 60 minutes. The sessions were tailored to each patient and focused on physical, occupational and speech therapy.
-
Monitoring: All patients were followed for a year, with visits scheduled at baseline, 3 months, 6 months and a year.
The results:
-
Safety: There were no severe adverse events related to the treatment. Overall, the adverse event rate was lower in the IV group than in the IT group, where patients experienced more procedure-related pain and headaches.
-
Improvements at 6 months: The IV group demonstrated statistically significant improvements in neurological deficits (NIHSS scores), functional independence, and quality of life compared to the control group. The IT group also showed an improvement compared to the control group, although not as significant.
-
Improvements at 12 months: Both the IV and IT groups showed statistically significant improvements compared to the control group. Researchers hypothesised that IT administration would be more effective than IV, but the study results did not support this assumption – there was no statistically significant difference between the two methods. Larger studies are needed to confirm the results and draw more accurate conclusions.[10]
What are the next steps?
Future studies should focus on optimising the dosage and frequency of the treatment, as well as determining whether any particular patient profile benefits especially well from the treatment. Larger-scale clinical trials will also be necessary to confirm the findings of any smaller-scale trial such as this one.
This research, as well as many other such trials investigating stem cell treatments, could come to fruition during your baby’s lifetime. Having access to as many sources of stem cells as possible could be key for them to access such treatments, particularly for conditions such as stroke which can strike very suddenly. To learn more about how you could preserve a rich source of stem cells for your baby as soon as they are born, complete the form below to request our free welcome pack.
References
[7] Stroke Association (2024). Understanding recovery. https://www.stroke.org.uk/stroke/recovery