Today marks World Cord Blood Day—a day dedicated to highlighting the medical breakthrough that began 36 years ago, in 1988, with a single transplant. That cord blood transplant opened the door to a new era in medicine. Since then, stem cells from cord blood have transformed countless lives, offering hope to those battling over 80 serious diseases including leukaemia, sickle cell anaemia, lymphoma, and more.
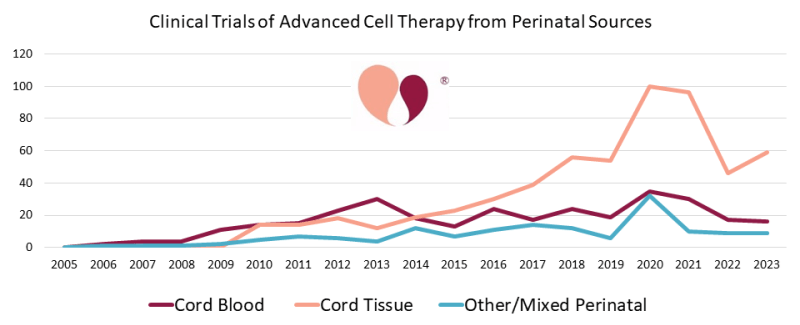
Once dismissed as medical waste, cord blood’s potential to heal is becoming more and more recognised, with over 60,000 transplants since 1988. Today, stem cells are the key players in regenerative medicine, studied in thousands of labs and clinical trials around the world. Scientists are exploring their potential to treat conditions as varied as bone fractures, spinal cord injuries, arthritis, and even Crohn’s disease.
Yet, despite this remarkable potential, too often cord blood is still discarded after birth, lost forever. This is why World Cord Blood Day was created: to shine a light on the therapeutic power of cord blood and to encourage more families to preserve this incredible resource for the future.
As research has continued though, it is no longer just cord blood that holds such promise, but also the cord tissue and placental stem cells which hold immense potential in regenerative medicine.
Cord blood news
A lot has happened in the cord blood field since last year. Here are some news you may want to catch up on if you’ve missed them…
-
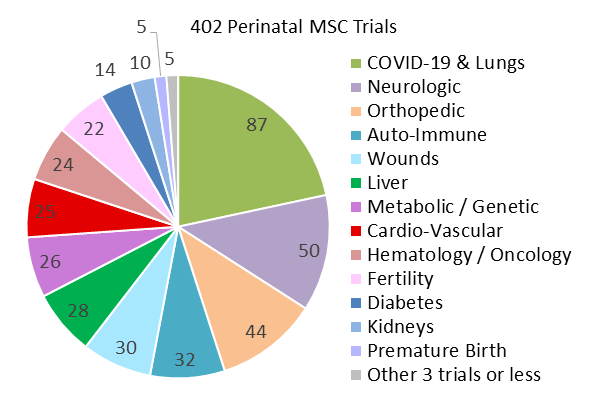
Researchers in China found that umbilical cord stem cells could aid in healing intestinal ulcers caused by Crohn’s disease.
-
A study found that umbilical cord stem cell therapy could improve ovarian function, a potentially important step towards overcoming the ‘biological clock’ of waning fertility.
-
A five-year-old boy with a rare genetic disorder received a life-changing transplant of cord blood stem cells that had been stored by the NHS for 15 years.
-
A clinical trial investigating the use of umbilical cord stem cells to treat chronic heart failure is underway.
-
Umbilical cord stem cells are being researched as a treatment for acute liver failure.
-
A new therapy could improve treatment outcomes for patients with Krabbe disease following a stem cell transplant.
-
A recent report by the Parents’ Guide to Cord Blood Foundation highlighted continued interest in treatments based on umbilical cord stem cells in the medical research field.
-
Haplo cord blood transplants, combining stem cells from a cord blood unit and a bone marrow donor, improve survival rates post-transplant and reduce the risk of graft-versus-host disease.
-
Umbilical cord exosomes could be used in developing life-changing therapies for a variety of conditions.
How can I bank my baby’s cord blood?
If you want to save this precious resource rather than having it thrown away, both public and private banking are available options.