This week we are learning about muscular dystrophy and how cord blood stem cells could help sufferers.
Muscular Dystrophy, also known as MD, is a hereditary condition which causes muscle weakness. It is a progressive condition which means those with muscular dystrophy deteriorate as time goes by.
There are several kinds of muscular dystrophy:
•Duchenne muscular dystrophy
•Myotonic dystrophy
•Facioscapulohumeral muscular dystrophy
•Becker muscular dystrophy
•Limb-girdle muscular dystrophy
•Oculopharyngeal muscular dystrophy
•Emery-Dreifuss muscular dystrophy [1]
While muscular dystrophy tends to affect both sexes equally there are a couple of exceptions. In the case of Duchenne muscular dystrophy, also known as DMD, boys are mainly affected. However girls can be affected but they have a milder form [1].
Becker muscular dystrophy, also known as BMD, is similar to Duchenne in the fact that it affects more boys than girls. BMD also affects similar areas of the body; however, the symptoms tend to be less severe [1].
Thankfully Duchenne and Becker muscular dystrophy is rare, affecting just 233 out of 1.49 million males in Northern England in 2009 [2].
Muscular dystrophy tends to run in families. It is usually caused by inheriting a faulty gene from one or both parents [3]. The faulty genes affected are those responsible for healthy muscle structure and function. In those with MD, the faulty genes mean that the cells which would normally maintain muscles are no longer able to do so which leads to muscle weakness and progressive disability [3].
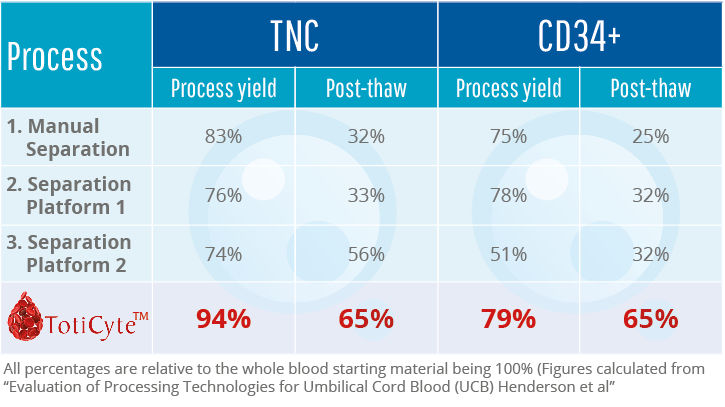
Unfortunately there is no cure for any kind of muscular dystrophy, current treatments aims to slow the progression of the illness [4]. However, stem cell researchers are investing the role of cord blood in patients with MD. One study took stem cells from umbilical cord blood and combined them with myoblasts from a patient with DMD. The authors of the paper concluded that “Our findings showed that umbilical cord blood CD34+ stem cells have the potential to interact with dystrophic muscle cells restoring the dystrophin expression of DMD cells in vitro. Although utilized within the context of DMD, the results presented here may be valid to other muscle-related therapy applications.” [5].
[1] http://www.nhs.uk/Conditions/Muscular-dystrophy/Pages/Symptoms.aspx
[2] http://www.cdc.gov/ncbddd/musculardystrophy/facts.html
[3] http://www.nhs.uk/Conditions/Muscular-dystrophy/Pages/Causes.aspx
[4] http://www.webmd.com/children/understanding-muscular-dystrophy-treatment
[5] http://www.translational-medicine.com/content/pdf/1479-5876-7-6.pdf