Stem Cell Blog
Употребата на матичните клетки од папочна врвца рапидно се зголемува. Пред 10 години крвта од папочна врвца можеше да лекува околу 40 состојби, но денес таа бројка е над 80. Со нетрпение очекуваме нови терапии за болести и нарушувања како што се дијабет, аутизам и мозочен удар, можете да бидете во тек со најновите случувања во регенеративната медицина на нашиот блог за матични клетки.
04/12/2024 BlogStem Cell TherapiesUses for Cord Blood
Last month researchers at The Parent’s Guide to Cord Blood Foundation compiled a report about how perinatal stem cells were being employed in clinical trials from 2019 through to the end of 2023. [1]
Perinatal stem cells are those which are collected in and around the perinatal period: the period immediately before and after birth.
These include stem cells from cord blood, cord tissue, the placenta and amnion.
In this blog, we’ll summarise some of their key findings and discuss what they mean in deciding to store stem cells for your baby.
Increase in the number of perinatal stem cell trials, despite COVID-19
In their report, researchers led by Dr Frances Verter point out how clinical trials using umbilical cord mesenchymal stem cells in particular reached a peak in 2020 and 2021, the result of accelerated research to help combat the COVID-19 pandemic.
They estimate that during the pandemic (2020-2022), nearly 41% of all advanced cellular therapy trials for COVID-19 relied on perinatal stem cells.
While the number of trials declined by almost half in the years that followed – to be expected, considering the impact of the pandemic on trial numbers – the researchers found that during the two years since their last report in 2021, the cumulative number of trials for advanced cellular therapies using perinatal stem cells increased by 17%.
This shows that the number of clinical trials using perinatal stem cells has not only returned to pre pandemic levels, but has actually increased, demonstrating a sustained interest in the clinical and therapeutic application of perinatal stem cells.
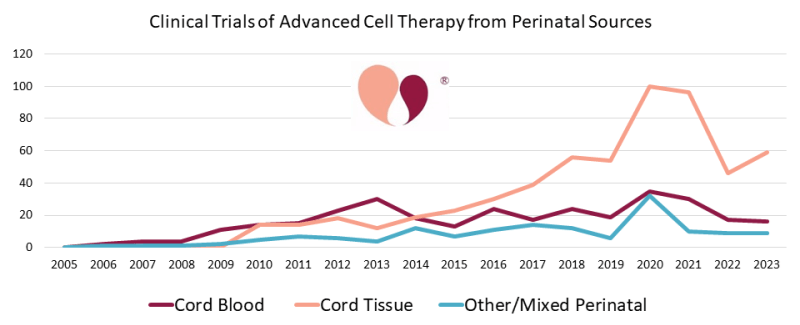
(graph courtesy of The Parents Guide to Cord Blood Foundation, https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells)
Trials for stem cells derived from placenta and amnion
Dr Verter and her team also point out that there are increasingly prominent roles for perinatal stem cells derived from a variety of sources beyond cord blood and cord tissue, namely: placenta and amnion.
Of the 402 clinical trials focusing on the use of mesenchymal stem cells derived or expanded from perinatal tissues, 9% utilised either placenta, amniotic membrane, or a mixture of a number of different perinatal stem cell sources. For reference, only 4% of trials derived MSCs from cord blood.
These numbers suggest that the placenta and amnion are becoming increasingly pivotal to the development of advanced cellular therapies using perinatal sources of stem cells, with the majority of these MSC trials focusing on COVID-19, neurological conditions, orthopaedic conditions and auto-immune disorders.
Cord tissue trials outpace cord blood trials
Since their last report on the cumulative number of trials through to the end of 2021, Dr Verter and her team found that in the years since, through to the end of 2023, there were 117 new trials utilising cord tissue and 40 new trials utilising cord blood. [2]
A key source of mesenchymal stem cells – which have the ability to differentiate into other specialised cell types such as muscle, nerve, and cartilage cells – cord tissue has once again shown itself to be at the forefront of trials utilising perinatal stem cells.
Of the 402 perinatal stem cell trials using MSCs, 87% of these utilised MSCs derived from cord tissue alone.
Considering that during the period from 2019-2023, over 75% of all perinatal stem cell trials were focused on the application of mesenchymal stem cells, cord tissue continues to be a vital source of the kind of stem cells that are driving current therapeutic interest in the application of stem cells from perinatal tissues.
Wide array of medical uses for perinatal mesenchymal stem cells
Another significant finding in this report is the sheer array of diagnosis categories that perinatal mesenchymal stem cells are being trialled for.
While around 45% of trials using perinatal mesenchymal stem cells focused on how they might be applied to treat COVID-19 and other respiratory illnesses, as well as neurological and orthopaedic conditions, another 46% of the total number of perinatal mesenchymal stem cell trials were divided across a wide range of medical diagnoses.
These medical diagnoses spanned trials for auto-immune disorders, the treatment of different forms of wounds, liver conditions, metabolic and genetic conditions (such as Krabbe disease and Hurler’s syndrome), cancers and blood cancers, and cardio-vascular conditions.
These figures suggest not only an increase in the number of perinatal mesenchymal stem cell trials, but also a broad spectrum of possible treatment applications, making them invaluable in the development of future advanced cellular therapies.
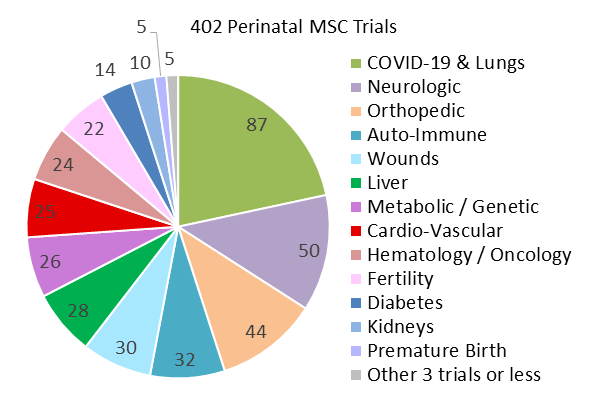
(graph courtesy of The Parents Guide to Cord Blood Foundation, https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells)
What does this mean for cord blood banking?
If you’re considering storing stem cells for your baby, the findings of this report are encouraging.
The sustained growth in clinical trials using perinatal stem cells, even beyond the pandemic, highlights the continued and expanding interest in their therapeutic potential.
Cord tissue, in particular, stands out as a critical source of mesenchymal stem cells, which are increasingly being used in a wide range of medical applications, from COVID-19 and neurological conditions to auto-immune disorders and orthopaedic treatments.
The growing use of placental and amniotic stem cells further emphasises the value of preserving these additional perinatal tissues, providing a great chance to maximise your baby’s ability to access future treatments.
With ongoing advancements in cellular therapies and the broad spectrum of diseases being targeted, banking stem cells from your baby’s umbilical cord and placenta could offer valuable opportunities for future medical treatments that go beyond what is available today.
Your baby’s stem cells may play a crucial role in the next generation of medical breakthroughs.
If you’re interested in storing stem cells for your baby, fill out the form below to request a free Welcome Pack. It contains information that will help to shed light on the collection process, our storage services, and the future potential offered by umbilical cord stem cells.
References
[1] Verter, F., Bersenev, A., & Couto, P. S. (2024, September 10). 2024 Update: How Many Clinical Trials Employ Perinatal Sources of Stem Cells? Parents Guide to Cord Blood Foundation. https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells
[2] Verter, F. (2022, September 15). 2022 Update: How many clinical trials use cord blood or cord tissue? Parents Guide to Cord Blood Foundation. https://parentsguidecordblood.org/en/news/2022-update-how-many-clinical-trials-use-cord-blood-or-cord-tissue
A new therapy, recently granted a UK Innovation Passport Designation, could help to improve treatment outcomes for Krabbe disease patients post-stem cell transplant.
What is Krabbe disease?
Krabbe disease is a rare genetic disorder affecting around 1 in every 100,000 births and is caused by a deficiency of the enzyme galactocerebrosidase (GALC), leading to the breakdown of the myelin in the nervous system.
The most common variant of Krabbe disease, Infant Krabbe Disease, affects children under the age of 1, and can cause muscle stiffness, seizures, and developmental delays. It is often fatal if untreated.
Approximately 85% of Krabbe disease cases are the infantile subtypes. [1]
What are the current treatment options for Krabbe disease?
Currently, the only effective treatment option for Krabbe disease is a transplant of haematopoietic stem cells (HSCs), which are found in bone marrow, peripheral blood, and umbilical cord blood. [2]
By transplanting HSCs from a donor to a Krabbe disease patient, the patient’s unhealthy cells lacking in the GALC enzyme are eventually replaced by healthy red blood cells, white blood cells and platelets derived from HSCs.
These healthy blood cells can then work to populate the brain with GALC enzyme activity, reducing the breakdown of myelin and thereby stabilise cognitive function. [3]
Stem cell transplants using haematopoietic stem cells from cord blood, specifically, have been shown to be highly effective in improving neurological outcomes if the transplant is performed before the development of symptoms. [4]
While HSCT remains the only viable treatment option for Krabbe disease, it is not a cure.
It also does not combat the peripheral neuropathy occasioned by Krabbe disease, a condition affecting the nerves beyond the brain and spinal cord, leading to decline in motor function. [5]
What is the new gene therapy and how does it improve stem cell transplant outcomes?
Developed by Forge Biologics, the FBX-101 therapy works by delivering a copy of the GALC gene to cells in the nervous system, which improves myelination (the process by which the myelin sheath forms) and, crucially, motor function.
It is designed to be administered intravenously after the current standard of care, a haematopoietic stem cell transplant.
In its early phase trial, REKLAIM, FBX-101 was shown to improve motor function in all five of the patients who underwent treatment.
Building on these promising results, the Innovation Passport designation means that FBX-101 will be able to enter the Innovative Licensing and Access Pathway (ILAP), which accelerates both market and regulatory access in the UK. [6]
Why is newborn screening for Krabbe disease so important?
Newborn screening for Krabbe disease is crucial because the condition progresses rapidly, especially in its infantile form, and early intervention is the key to preventing severe neurological damage.
Ideally, the patient would receive a transplant within 30 days in order to have the best chance of improved neurological and transplant outcomes. [7]
Symptoms of Krabbe disease often appear within the first few months of life, and once they start, the deterioration of the nervous system is fast and irreversible.
By the time symptoms are noticeable, significant damage has already occurred, limiting the effectiveness of available treatments.
Newborn screening allows for early diagnosis before symptoms develop, enabling early intervention through HSCT, which is at its most effective if administered before significant damage to the nervous system. [8]
Could cord blood banking help?
Umbilical cord blood is a vital source of haematopoietic stem cells which can differentiate into various kinds of blood cells. These cells are crucial in the treatment of Krabbe disease, but rely on finding a donor match in order for a transplant to be successful.
If Krabbe disease runs in your family, saving cord blood for every child is probably a worthwhile investment.
If your baby does end up developing Krabbe disease, having their sibling’s stem cells in storage could make the difference in being able to access a life-saving transplant as a sibling has a 75% chance of being a partial donor match.
For more information about how cord blood banking could help with the treatment of Krabbe disease, visit our Krabbe Disease and Stem Cells page, here.
If either you or a family member or someone you know is expecting, why not download our free Welcome Pack to learn more about the benefits of cord blood banking. Simply fill out the form below.
References
[1] Isabel C. Yoon, Nicholas A. Bascou, Michele D. Poe, Paul Szabolcs, Maria L. Escolar; Long-term neurodevelopmental outcomes of hematopoietic stem cell transplantation for late-infantile Krabbe disease. Blood 2021; 137 (13): 1719–1730. doi: https://doi.org/10.1182/blood.2020005477
[2] Isabel C. Yoon, Nicholas A. Bascou, Michele D. Poe, Paul Szabolcs, Maria L. Escolar; Long-term neurodevelopmental outcomes of hematopoietic stem cell transplantation for late-infantile Krabbe disease. Blood 2021; 137 (13): 1719–1730. doi: https://doi.org/10.1182/blood.2020005477
[3] (2022, August 13). Krabbe Disease (Globoid Cell Leukodystrophy). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/6039-krabbe-disease-globoid-cell-leukodystrophy
[4] Wright, M. D., Poe, M. D., DeRenzo, A., Haldal, S., & Escolar, M. L. (2017). Developmental outcomes of cord blood transplantation for Krabbe disease: A 15-year study. Neurology, 89(13), 1365–1372. https://doi.org/10.1212/WNL.0000000000004418
[5] Beltran-Quintero, M.L., Bascou, N.A., Poe, M.D. et al. Early progression of Krabbe disease in patients with symptom onset between 0 and 5 months. Orphanet J Rare Dis 14, 46 (2019). https://doi.org/10.1186/s13023-019-1018-4
[6] (2024, March 19). Forge Biologics’ Novel AAV Gene Therapy FBX-101 for Patients with Krabbe Disease is Granted UK’s Innovation Passport Designation. Forge Biologics. https://www.forgebiologics.com/forge-biologics-novel-aav-gene-therapy-fbx-101-for-patients-with-krabbe-disease-is-granted-uks-innovation-passport-designation/
[7] Page, K. M., Ream, M. A., Rangarajan, H. G., Galindo, R., Mian, A. Y., Ho, M. L., Provenzale, J., Gustafson, K. E., Rubin, J., Shenoy, S., & Kurtzberg, J. (2022). Benefits of newborn screening and hematopoietic cell transplant in infantile Krabbe disease. Blood advances, 6(9), 2947–2956. https://doi.org/10.1182/bloodadvances.2021006094
[8] Page, K. M., Ream, M. A., Rangarajan, H. G., Galindo, R., Mian, A. Y., Ho, M. L., Provenzale, J., Gustafson, K. E., Rubin, J., Shenoy, S., & Kurtzberg, J. (2022). Benefits of newborn screening and hematopoietic cell transplant in infantile Krabbe disease. Blood advances, 6(9), 2947–2956. https://doi.org/10.1182/bloodadvances.2021006094
One of the questions we get asked most by expectant parents is whether or not cord blood banking is ‘worth it’.
You may have heard about it online, or through a friend, but don’t necessarily know what it entails, or what the benefits are.
In this blog, we’ll break down everything you need to know—what cord blood banking is, why it matters, the benefits, costs, and whether it’s the right choice for your family.
What is cord blood banking?
Cord blood banking is the process of collecting and storing the precious blood from your baby’s umbilical cord, along with other vital perinatal tissues like the placenta, cord tissue, and amnion.
These tissues are rich sources of two powerful types of stem cell: haematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs), which both have huge therapeutic potential.
Haematopoietic stem cells (HSCs)
HSCs are found in cord blood, and have the ability to differentiate (transform) into all types of blood cells, including white blood cells, red blood cells and platelets. This ability makes HSCs well positioned for the treatment of blood disorders like sickle cell anaemia and leukaemia.
HSCs from cord blood are already being used primarily in donor treatments for more than 80 different conditions, including blood cancers like lymphoma, immune disorders like SCID, and blood disorders like aplastic anaemia.
Mesenchymal stem cells (MSCs)
MSCs are found in cord blood, cord tissue and placenta and have the ability to differentiate into many different types of cell, including cartilage, nerve, muscle, fat, and bone cells.
This plasticity makes them ideal for use in an emergent field of medical research called regenerative medicine. Excitingly, there are currently hundreds of clinical trials investigating the application of MSCs in therapies for diseases that are currently incurable, like stroke, heart failure, and Parkinson’s disease.
Why is having your baby’s own stem cells available important?
Stem cell therapy depends on the body’s immune system not rejecting the transplanted cells. When using publicly donated stem cells from a donor this means finding an HLA match (human leukocyte antigens, which are gene complexes that encode cell-surface proteins that help the immune system determine what does and doesn’t belong to the body) and using immuno-suppressive drugs to minimise the chances of rejection.
However, cord blood banking enables your baby to have their own perfectly matched stem cells ready and waiting in storage, meaning they can access therapies without the risk of rejection.
Is cord blood banking safe?
The cord blood collection process is completely safe, non-invasive, and takes place in a separate room after birth, handled by a licensed phlebotomist.
What are the benefits of cord blood banking?
Life Saving Treatments
Cord blood stem cells are a proven treatment option for over 80 life-threatening conditions. They have been used in more than 40,000 transplants worldwide, providing a vital alternative to bone marrow transplants for conditions like leukaemia, lymphoma, and sickle cell anaemia.
Protection for the Whole Family
By preserving your baby’s stem cells, you’re not only protecting your child’s future health but also potentially safeguarding the entire family. These stem cells are a perfect match for your baby, with a 1 in 4 chance of being a perfect match, and a 50% chance of being a partial match, for a sibling. Additionally, there’s always a 50% chance they could be a partial match for a parent as well.
Future Potential in Medical Research
Researchers are exploring the use of mesenchymal stem cells in the treatment of diseases like stroke, diabetes, and heart disease. Although these therapies are still in clinical trials, the potential for future applications is vast. By banking your baby’s umbilical cord and placenta now, you could unlock access to cutting-edge treatments in the future.
Why bank cord blood with Cells4Life?
Industry Leading Innovation
Our CellsPlus service uses our industry leading processing technology TotiCyte to retain 3 times the number of stem cells compared to other cord blood processing methods.
More cells in storage means more opportunities for treatments, and could make the difference between treating a child and an adult. Our CellsPlus service also means that cord blood banking is 100% compatible with delayed cord clamping for the first time.
Comprehensive Services
We’re the only UK cord blood bank offering the most comprehensive range of stem cell banking services, including cord blood, tissue, amnion and placenta banking. Saving a diverse range of cells for your baby maximises the range of treatment opportunities they’ll be able to access.
Dual location storage
We can store samples in multiple portions across two locations with SecurePlus. This means that your baby can use their samples multiple times, only using what they need and saving the rest. Dual location storage also provides the peace of mind of knowing that should anything happen at one location, their stem cells are still protected at the other.
Proven Track Record
We are the first choice for UK parents, with more UK families storing with us and over 150,000 samples in storage across our two Sussex sites.
Is cord blood banking worth it?
It’s been predicted that 1 in 3 of us will require some sort of regenerative therapy within our lifetimes. [1] Your baby might be part of the first generation to live beyond 100. Imagine the range of stem cell therapies that could become available to them within their lifetime. Saving their stem cells gives them the best chance of accessing these new and emerging therapies.
Cord blood banking is probably also worth doing if you have a history of illness in your family. Your baby’s stem cells may even end up being the key to safeguarding them, or a close family member, against life-altering conditions that remain all too prevalent; conditions like arthritis, diabetes, cancer, and heart disease.
Your baby’s stem cells could change their life one day.
References
[1] Regenerative Medicine. Association for the Advancement of Blood & Biotherapies. https://www.aabb.org/news-resources/resources/cellular-therapies/facts-about-cellular-therapies/regenerative-medicine#:~:text=Regenerative%20medicine%20also%20may%20enable,potentially%20benefit%20from%20regenerative%20medicine.
Five-year-old Gunner Lewis-Vale from Shropshire is finally able to step outside and enjoy the summer for the first time in six months, thanks to a successful stem cell transplant from umbilical cord blood donated 15 years ago. [1] [2] [3]
Gunner’s Story
At just 17 months old, Gunner was diagnosed with mucopolysaccharidosis type I Hurler syndrome, a rare genetic disorder affecting the body’s ability to break down sugars. His family were told that without a transplant he would have only a year or two to live.
After undergoing a failed transplant using stem cells from a donor in Germany, Gunner and his family desperately sought another solution.
Remarkably, stem cells donated to NHS Blood and Transplant in 2008 were found to be a match for Gunner. Derived from umbilical cord blood, these cells had been cryogenically stored in liquid nitrogen for 15 years, ready and waiting to be used in a life-changing transplant.
In January, Gunner received the stem cell transplant, which aimed to provide him with the ability to produce the enzyme he lacked in order to break down sugars.
When the body is unable to break down sugars, these build up in what’s known as lysosomes, parts of the cell responsible for waste management. [4]
The toxic buildup of waste molecules in lysosomes can have dramatic effects, leading to the cells either dying or not being able to function properly. This in turn causes severe symptoms, including problems with the heart, hearing loss, enlarged organs, respiratory problems and hernias.
Due to the nature of the transplant, Gunner was forced to isolate for six months in order to avoid infection while his new white blood cells (derived from the cord blood stem cell transplant) were given the chance to propagate.
Six months on and Gunner is reportedly enjoying the summer months with his big sister Daisy, going to the park, feeding the ducks, and getting back to being a five-year-old boy.
Gunner’s family are elated to see his new lease of life and are helping to raise awareness of the importance of stem cell donation and the power of cord blood stem cells to change lives.
Cord blood banking and the importance of a match
Gunner’s story highlights the importance of being able to access a stem cell donor match.
Gunner was fortunate enough to find a match with umbilical cord blood stem cells that had been donated through NHS Blood and Transplant.
Storing your baby’s stem cells privately however, gives them access not only to their own perfectly matched stem cells, but also a 75% chance that they may be usable by a sibling.
As the field of regenerative medicine continues to advance, huge strides are being made in autologous stem cell treatments for genetic disorders. Autologous stem cell treatments are ones where a patient’s own stem cells are used.
Gene editing technologies like CRISPR offer huge potential in the development of autologous stem cell therapies for inherited conditions currently requiring transplants. [5]
In November last year we reported on a new autologous therapy approved by the UK regulator for sickle cell disease and beta thalassemia.
Previously only treatable with a stem cell transplant from a donor, these two inherited diseases were found to be curable with stem cells taken from patients which were then edited to have the faulty, disease-causing genes removed. [6]
There are many therapies currently in development to treat inherited diseases with autologous stem cells, diseases ranging from immunodeficiencies to blood disorders and metabolic disorders. [7]
By saving your baby’s own stem cells, you could give them a better chance of accessing these therapies should they ever need one in future.
To find out more about how cord blood banking could safeguard your baby’s health, fill out your details below for a free Welcome Pack.
References
[1] Fofana, A. (2024, July 20). Boy, 5, saved by stem cell transplant. BBC. https://www.bbc.co.uk/news/articles/c4ngl620j1lo
[2] (2024, July 20). Family of Shropshire boy, 5, with rare disorder given hope after umbilical cord transplant. ITV News. https://www.itv.com/news/central/2024-07-20/family-of-boy-5-with-rare-disorder-given-hope-after-umbilical-cord-transplant
[3] Lynch, N. (2024, July 20). Boy, 5, diagnosed with deadly rare condition has life transformed after stem cell transplant from umbilical cord blood. Sky News. https://news.sky.com/story/boy-diagnosed-with-deadly-rare-condition-has-life-transformed-after-stem-cell-transplant-from-umbilical-cord-blood-13181740
[4] (2022, August 17). Hurler Syndrome. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/24000-hurler-syndrome
[5] Qiu, Hou-Yuan et al. “Current advances of CRISPR-Cas technology in cell therapy.” Cell insight vol. 1,6 100067. 26 Oct. 2022, doi:10.1016/j.cellin.2022.100067
[6] NHS England (2023, December 8). Casgevy – how it works. Genomics Education Programme. https://www.genomicseducation.hee.nhs.uk/blog/casgevy-how-it-works/
[7] Staal, Frank J T et al. “Autologous Stem-Cell-Based Gene Therapy for Inherited Disorders: State of the Art and Perspectives.” Frontiers in pediatrics vol. 7 443. 31 Oct. 2019, doi:10.3389/fped.2019.00443
This year’s World Sickle Cell Day is on the 19th June, a day to recognise and raise awareness of the disease, the millions around the world who suffer from it, and ongoing research into how treatment is advancing.
With this year’s theme being ‘we are STRONGER TOGETHER’, we thought it would be a good opportunity to highlight how cord blood transplants between siblings have emerged as a viable treatment alternative for those suffering from the condition.
Making use of sibling cord blood necessitates having it in storage and so in celebration of World Sickle Cell day, we wanted to highlight how cord blood banking could provide a lifeline for those suffering from the disease, as well as how storing cord blood for your baby could help safeguard the health of your family.
What is sickle cell disease?
Sickle cell disease is the name for a group of inherited blood disorders that are passed down from parents to children.
Particularly common amongst those who have African or Caribbean heritage, sickle cell disease inhibits the haemoglobin in red blood cells from carrying oxygen.
This can lead to the red blood cells in those with the condition to become misshapen, inflexible and liable to sticking together and blocking blood flow, causing tremendous pain – known as sickle cell crises – in addition to an increased risk of stroke, lung problems, eye problems and infection.
The disease gets its name from the shape of the red blood cells affected by the condition: crescent or ‘sickle’ shaped rather than discoid. [1]
What treatments are available for sickle cell disease?
Currently, treatments for sickle cell disease focus primarily on the alleviation of symptoms.
While there have been significant steps forward in recent years, including the development of the Casgevy therapy which utilises genetically engineered bone marrow stem cells from the patients themselves in lieu of a donor transplant, medicines like antibiotics and painkillers remain the most prevalent way of combating sickle cell.
There is only one known cure for sickle cell disease: a stem cell or bone marrow transplant. In these treatments, healthy red blood cells are produced by the donated stem cells, replacing the ones that are affected by sickle cell. [2]
However, difficulty in locating an unrelated donor match, in addition to the risks posed by graft-versus-host disease, hinders the ready availability of transplantation as a treatment option.
The benefits of cord blood banking for sickle cell disease
Within the last decade, sibling cord blood transplants have emerged as a viable alternative to bone marrow transplants as a treatment option for sickle cell disease.
A comprehensive study in 2017 following the success rates of sibling cord blood transplants over a period of 20 years found that of the 28 patients with sickle cell who received cord blood from a sibling, all but one are both alive and free from sickle cell disease. [3]
With a reduced risk of graft-versus-host disease, in addition to a 25% chance of a perfect match and a 50% chance of a partial match, using the stem cells from a sibling’s umbilical cord blood alleviates many of the current obstacles to obtaining a transplant to treat sickle cell disease.
Moreover, because of the way sickle cell is passed down between parents and children, if one child is born with sickle cell disease then there’s a 75% chance that a subsequent child will not have the disease, making a cord blood transplant between siblings possible. [4]
Should I store my baby’s cord blood?
Underlying the breakthroughs in treating sickle cell through a sibling cord blood transplant is one crucial detail: whether or not that sibling has cord blood samples in storage. There’s only one opportunity to save their cord blood: in the minutes after they’re born.
Without cord blood samples in storage, availability to stem cell transplant treatments for sickle cell, and other blood or inherited conditions, becomes more difficult as it’s harder to find a suitable match.
Ensuring that you save cord blood for every child maximises opportunities for treatment, particularly in instances where a sibling transplant could provide a cure for conditions requiring an HLA match, like sickle cell disease.
Additionally, with the emergence of the aforementioned Casgevy therapy and ongoing trials exploring the possibility for autologous stem cell treatments for sickle cell disease, saving your baby’s stem cells means that they have improved access to cutting edge therapies using their own cord blood samples. [5]
Storing cord blood for every child is the only way to ensure that they have improved access to the benefits of cord blood banking.
If you want to learn more about how storing cord blood for your baby could provide protection for their health and the health of their siblings, fill out the form below for a free Welcome Pack.
References
World Cancer Day takes place this year on 4th February. A day of global unity, dedicated to raising awareness about cancer, World Cancer Day also plays an important part in dispelling myths about cancer, in addition to promoting early detection and prevention.
This year’s World Cancer Day theme is ‘Close the Care Gap’, referring to the gap between the level of care received by privileged vs underprivileged cancer patients.
On this significant day, we’re invited not only to reflect on the impact of cancer but also asked to consider how care outcomes for a cancer diagnosis could be improved.
One such way is through cord blood banking, which is already being used in over 80 treatments, including for leukaemia.
In this blog, we will delve into the importance of cord blood banking and how it is offering hope in the fight against cancer.
Understanding Cord Blood Banking
Cord blood banking involves the collection and preservation of the residual blood from the newborn umbilical cord following birth.
This precious resource contains powerful stem cells that can develop into various specialised cells, such as the ones in hair, skin, organs, blood and the nervous system.
Their unique abilities to self-replicate and differentiate positions them at the forefront of regenerative medicine, a branch of medicine that makes use of stem cells’ potential capacity to repair, renew and regrow cells and tissues to treat a range of diseases. [1]
The Benefits of Cord Blood Banking
Cord blood stem cells are the approved therapy for over 80 diseases, including leukaemia, neuroblasts, and certain genetic disorders.
Their relative naivety and plasticity when compared to stem cells derived from other sources makes them some of the purest and most powerful forms of stem cell available.
Cord blood stem cells are a 100% match for your baby, meaning that they can be used in therapies without risk of rejection. They also have a good chance of being a perfect match for siblings and a partial match for family members, offering a safer and more accessible option for transplantation.
A painless and non-invasive procedure, cord blood collection is safe, non-invasive and poses little to no risk to the mother or baby.
As medical research advances, the potential uses of cord blood stem cells continue to expand.
Researchers are exploring their use in regenerative therapies that seek to harness the power of these stem cells in order to combat diseases that are currently incurable, including some forms of cancer. [2]
Promoting Cord Blood Banking on World Cancer Day
World Cancer Day provides an ideal platform to educate expectant parents and the general public about some of the most pioneering research happening to combat cancer, amongst them: cord blood banking.
Understanding the potential lifesaving impact of this resource is the first step in motivating more families to consider this option.
World Cancer Day reminds us of the global challenge posed by this disease, but it also presents an opportunity to promote hope and innovative solutions.
Cord blood banking is one such solution that has the potential to save lives and help in the battle against cancer.
Sarah’s Story
For eight year old Sarah, for instance, cord blood banking was the last hope she had after both chemotherapy and a bone marrow transplant proved ineffective in the treatment of her acute myeloid leukaemia. [3]
A form of cancer that attacks the monocyte or granulocyte cells, naive progenitor white blood cells from bone marrow, acute myeloid leukaemia predominantly affects children and young people.
Chances of a full recovery are rarely good.
Having undergone a bone marrow transplant from her brother, Sarah initially showed promising signs of recovery, until the cancer returned.
Rounds of emergency chemotherapy were required to try to keep the cancer at bay, but it continued to return.
Seeing no other option for Sarah, doctors at the Royal Manchester Children’s Hospital offered her a pioneering stem cell transplant using donated cord blood.
Incredibly, thanks to this treatment Sarah and five other children who also participated in the trial, are now in remission; their access to a healthy, happy life restored to them.
Although this transplant was the result of donation, privately banking cord blood stem cells means that your baby always has access to their own perfect donor match: themselves.
This drastically reduces the risk of rejection should they ever need to access a therapy in future like Sarah’s.
With thousands of clinical trials currently underway to explore the potential uses for umbilical cord blood stem cells in a range of regenerative treatments, storing these precious cells the day baby is born could safeguard their future for years to come.
For more information about the power of cord blood banking, download your FREE Welcome Pack below.
Sources
22/01/2024 BlogNewsPregnancy AdviceUses for Cord Blood
November 15th is World Cord Blood Day. This annual event was created to raise awareness of cord blood, what it is and some of the therapeutic benefits it can offer.
If you are curious to find out more, read on.
16/01/2024 BlogNewsUses for Cord Blood
A recent study has suggested that therapeutic interventions such as umbilical cord blood stem cell therapy, which impact immune modulation and regulation of neural connectivity, have shown great promise in the treatment of autism.
16/01/2024 BlogUses for Cord Blood
















