Stem Cell Blog
Употребата на матичните клетки од папочна врвца рапидно се зголемува. Пред 10 години крвта од папочна врвца можеше да лекува околу 40 состојби, но денес таа бројка е над 80. Со нетрпение очекуваме нови терапии за болести и нарушувања како што се дијабет, аутизам и мозочен удар, можете да бидете во тек со најновите случувања во регенеративната медицина на нашиот блог за матични клетки.
England flanker Tom Curry is undergoing stem cell therapy as a follow-up to last year’s career-saving surgery.[1]
Suffering from chronic hip pain and reduced range of motion, Curry was diagnosed with femoroacetabular impingement syndrome, where the ball of the hip joint is abnormally shaped, causing uneven wear and tear in the joint resulting in cartilage and bone damage.[2][3]
In Curry’s case, there was what was defined as an arthritic change within the hip[4] – labrum and cartilage tears, as well as abnormal bone growth. This was corrected in a six-hour surgery, which reshaped the ball of his hip and repaired the labrum and cartilage via a stem cell transplant.[2]
To fix the tears in Curry’s cartilage, leading hip surgeon Damian Griffin placed a synthetic cartilage graft in the joint and applied stem cells taken from Curry’s bone marrow to it to grow a new surface within the joint.[5] The procedure is performed arthroscopically (keyhole surgery), and it has a much shorter recovery time and carries less risk than surgeries involving metal implants, such as a hip resurfacing, where metal surfaces are used to cover the joint,[6] or a complete hip replacement.[7]
Now, Curry is undergoing another stem cell therapy in a bid to make it to the 2027 Rugby World Cup without needing more surgery.[1] There are fewer details available about this therapy, but it has been stated to be a stem cell injection in his hip to help bone growth.
How can stem cells help with injury recovery?
Stem cells possess remarkable regenerative potential, which therapies and procedures like those Curry is undergoing take advantage of. The cells that make up bone and cartilage typically derive from mesenchymal stem cells (MSCs), which, in addition to their ability to turn into a variety of specialised cell types, also have anti-inflammatory properties. This makes them ideal to help repair damaged tissue, particularly cartilage, which has very limited regenerative capacity of its own.
Curry is far from the only elite athlete to turn to stem cells to get back to form. Footballer Cristiano Ronaldo used stem cell therapies to successfully address knee problems[8], while tennis great Rafael Nadal treated both chronic knee issues and a long-standing back complaint[8][9]. Boxing legend Mike Tyson also had stem cell therapy.[8]
To find out more about the regenerative power of stem cells, and how your baby’s umbilical cord stem cells could safeguard their health for life, simply fill in the form below to request a free information pack.
References
04/12/2024 BlogNewsStem Cell NewsUses for Cord Blood
Today marks World Cord Blood Day—a day dedicated to highlighting the medical breakthrough that began 36 years ago, in 1988, with a single transplant. That cord blood transplant opened the door to a new era in medicine. Since then, stem cells from cord blood have transformed countless lives, offering hope to those battling over 80 serious diseases including leukaemia, sickle cell anaemia, lymphoma, and more.
Once dismissed as medical waste, cord blood’s potential to heal is becoming more and more recognised, with over 60,000 transplants since 1988. Today, stem cells are the key players in regenerative medicine, studied in thousands of labs and clinical trials around the world. Scientists are exploring their potential to treat conditions as varied as bone fractures, spinal cord injuries, arthritis, and even Crohn’s disease.
Yet, despite this remarkable potential, too often cord blood is still discarded after birth, lost forever. This is why World Cord Blood Day was created: to shine a light on the therapeutic power of cord blood and to encourage more families to preserve this incredible resource for the future.
As research has continued though, it is no longer just cord blood that holds such promise, but also the cord tissue and placental stem cells which hold immense potential in regenerative medicine.
Cord blood news
A lot has happened in the cord blood field since last year. Here are some news you may want to catch up on if you’ve missed them…
-
Researchers in China found that umbilical cord stem cells could aid in healing intestinal ulcers caused by Crohn’s disease.
-
A study found that umbilical cord stem cell therapy could improve ovarian function, a potentially important step towards overcoming the ‘biological clock’ of waning fertility.
-
A five-year-old boy with a rare genetic disorder received a life-changing transplant of cord blood stem cells that had been stored by the NHS for 15 years.
-
A clinical trial investigating the use of umbilical cord stem cells to treat chronic heart failure is underway.
-
Umbilical cord stem cells are being researched as a treatment for acute liver failure.
-
A new therapy could improve treatment outcomes for patients with Krabbe disease following a stem cell transplant.
-
A recent report by the Parents’ Guide to Cord Blood Foundation highlighted continued interest in treatments based on umbilical cord stem cells in the medical research field.
-
Haplo cord blood transplants, combining stem cells from a cord blood unit and a bone marrow donor, improve survival rates post-transplant and reduce the risk of graft-versus-host disease.
-
Umbilical cord exosomes could be used in developing life-changing therapies for a variety of conditions.
How can I bank my baby’s cord blood?
If you want to save this precious resource rather than having it thrown away, both public and private banking are available options.
Public banking means the cord blood stem cells are stored in a cord bank that makes them accessible to anyone who might need them. The NHS public cord bank accepts donations if you are giving birth at one of three hospitals; the Anthony Nolan charity public cord bank accepts donations from a further five hospitals.
Alternatively, you can choose to bank your baby’s cord blood privately, storing the stem cells solely for your family’s own use. They will be ready and waiting should your baby ever need them for treatment, and could be useful for family members, too – there is a 25% chance they would be an exact match for a sibling, or 75% chance of a partial match. They are also a guaranteed partial match for parents.
Everything about our services has been tailored to provide the maximum potential benefit to parents who store their baby’s stem cells with us, such as our advanced processing technology that retains up to three times more stem cells than industry-standard processing methods, meaning full compatibility with delayed and optimal cord clamping. We are also the only UK cord blood bank to offer placenta and amnion storage.
To learn more about cord blood banking and why most UK parents choose to store with us, simply fill in the form below for a free welcome pack.
The results reported from Phase II of the first FDA-approved trial for the treatment of multiple sclerosis (MS) using stem cells are highly promising, suggesting that stem cells could be a viable treatment option to help improve the lives of those with the condition. [1]
What is the MS trial?
The Phase II trial, which was carried out by The Tisch MS Research Center of New York, constitutes the next stage in the development of the groundbreaking research signalled by the results from Phase I, the first FDA-approved trial to explore the injection of stem cells for MS.
The Phase II trial involved 54 patients split between a test group and a control group in a randomised, double-blind, placebo-controlled study.
Members of each group received 6 injections of either autologous (meaning their own) mesenchymal stem cell-derived neural progenitors (MSC-NPs) or saline placebo every two months.
These injections were administered into the cerebrospinal fluid of multiple sclerosis patients.
The study utilised a cross-over model by which patients who received the stem cell injections in year 1 were then given the saline placebo in year 2 and vice versa.
How does the stem cell treatment work?
Building on their findings from Phase I, researchers identified MSC-NPs for the treatment having ascertained that they promote tissue regeneration and immunomodulatory effects, in addition to being safe and well tolerated. [2]
MSC-NPs are a subpopulation of mesenchymal stem cells that can upregulate growth factors like hepatocyte growth factor (HGF), and minimise ectopic differentiation – essentially, the abnormal differentiation of cells.
By injecting them into the cerebrospinal fluid – a process called intrathecal (IE) injection – researchers found in an experimental autoimmune encephalomyelitis (EAE – an accepted way of modelling the effects of MS) mouse model that MSC-NPs were associated with increased spinal cord myelination, neurological recovery and reduced immune infiltration into the central nervous system. [3]
What were the results?
The results of the Phase II trial demonstrated huge promise for the use of stem cells in treating MS.
Patients requiring walking assistance saw significant improvements in both a timed 25-foot walk test and a 6 minute walking test than those in the control group.
Additionally, treatment recipients demonstrated improved bladder function, with 69% showing improvements in post-void residual volume.
Amongst the other findings were indicators that these stem cells could be helping to restore neuronal cells and reverse cognitive decline in patients with less advanced disease progression.
Furthermore, the stem cell treatment occasioned notable biomarker changes in cerebro-spinal fluid, especially with regards to the decreased levels of CCL2, a protein associated with inflammation, and the increased levels of MMP9, an indicator of the increased presence of reparative cells. [4]
Overall these findings are extremely promising, indicating that stem cells could be used in future treatments that may help to reverse many of the most debilitating aspects of multiple sclerosis, like disability.
The next stage in the study will be for researchers to investigate the effects of increasing the stem cell dosage.
What does this mean for cord blood banking?
This trial is just the latest example of the regenerative potential stem cells have to help treat life-changing conditions like MS.
As exemplified by this study, mesenchymal stem cells in particular, with their immunomodulatory and tissue repair properties, are especially promising.
Incredibly, the umbilical cord and placenta are one of the richest sources of these stem cells, but are routinely thrown away after birth.
By saving these for your baby, you could be giving them the key to future therapies for everything from cancer and stroke to diabetes and heart disease.
The potential offered by stem cells is vast, but you only get one chance to save baby’s stem cells, and that’s the day they’re born.
To find out more about cord blood banking and how it could protect your family’s health, fill out the form below to request a free Welcome Pack.
References
[1] FDA-Approved Phase II Stem Cell Treatment Trial Shows Significant and Diverse Improvements for Multiple Sclerosis (MS) Patients. Tisch MS Research Centre of New York. https://www.tischms.org/phase-ii-analysis-results
[2] Harris, Violaine K. et al. (2018) Phase I Trial of Intrathecal Mesenchymal Stem Cell-derived Neural Progenitors in Progressive Multiple Sclerosis. eBioMedicine, Volume 29, 23 – 30. https://doi.org/10.1016/j.ebiom.2018.02.002
[3] Harris, Violaine K. et al. (2012) Clinical and pathological effects of intrathecal injection of mesenchymal stem cell-derived neural progenitors in an experimental model of multiple sclerosis. Journal of the Neurological Sciences, Volume 313, Issue 1, 167 – 177. https://doi.org/10.1016/j.jns.2011.08.036
[4] Harris, V.K., Stark, J., Williams, A. et al. (2024) Efficacy of intrathecal mesenchymal stem cell-neural progenitor therapy in progressive MS: results from a phase II, randomized, placebo-controlled clinical trial. Stem Cell Res Ther 15, 151 (2024). https://doi.org/10.1186/s13287-024-03765-6
04/12/2024 BlogStem Cell NewsStem Cell Therapies
New research has demonstrated the significant role stem cells play in skin and hair development, which could lead to revolutionary new anti-ageing treatments. [1]
By identifying the ways in which the body grows skin, researchers believe that their findings could lead to the use of artificial skin in treatments for burns, wounds, and age-related degeneration.
The research was conducted as part of The Human Cell Atlas project, which aims to map the genetic instructions contained in every cell in the human body to discover how they work.
New discoveries about skin formation
The study looked at the role immune cells, specifically macrophages, play in the development of skin during pregnancy.
While macrophages – which are a type of white blood cell responsible for killing pathogens – are primarily known for their importance as part of the immune system, researchers sought to identify how they contribute to skin formation in a process known as morphogenesis.
In order to do this, a so called ‘reference atlas’ of prenatal skin (that is, skin that forms between 7-17 weeks after conception) was made using advanced techniques including single cell and spatial transcriptomics – a study of RNA molecules within both one and a population of cells – to detail how elements both within and between skin cells interact.
Their findings showed that interactions between immune cells like macrophages and non-immune cells were crucial for key processes in morphogenesis, including hair follicle development, scarless wound healing, and the formation of blood vessels in the skin. [2]
The important role of stem cells in determining skin formation
Researchers were able to verify their findings about the significant role played by immune cells in skin morphogenesis by comparing pre-natal and adult skin with a lab-grown skin model derived from stem cells.
The model, known as an organoid, successfully mimicked many aspects of skin and hair follicle development found in prenatal and adult skin.
However, it was only when researchers added macrophages that they found the model created blood vessel networks, confirming that immune cells play a more significant role in the development of skin than previously thought.
This stem-cell derived model of human skin is thought to have a vast array of possible therapeutic applications extending from use in identifying the development of conditions affecting skin and hair to providing a more accurate test material for future skin and hair treatments. [3]
Mesenchymal stem cells – key players in hair and skin formation
Another area researchers looked at during the study was the formation of hair follicles during prenatal development.
In earlier studies with mice, researchers identified special cells called pre-Dc cells that eventually become part of the hair follicle structure (called the dermal condensate, or Dc). [4]
Researchers identified similar cells in human prenatal skin and tracked how they developed into the Dc and another structure called the dermal papilla (Dp), which is important for hair growth.
Using various advanced methods, researchers were able to map out the development of these cells over time and predict their paths.
They found that certain early skin cells (fibroblasts) go down one of two routes: some become specialised for hair follicle formation, while others develop into more general skin cells.
As the hair-specific cells move toward the outer layer of the skin, they turn on genes that help them stick together and form the structures needed for hair growth.
The study also looked at how mesenchymal cells interact with skin’s outer (epithelial) cells during hair follicle formation.
They identified important signalling molecules, such as CXCL12, that help guide cell migration and organisation. Interestingly, immune cells were also predicted to assist with these processes. [5]
Discovering the genetic origins of skin and hair conditions
Having mapped how skin and hair developed in pre-natal skin, researchers turned to investigating the origins of certain skin and hair conditions.
They found that reduced hair growth (hypotrichosis) and abnormal hair shapes (like pili torti) are caused by specific genes that are active during early hair follicle development.
Similarly, they were able to identify that epidermolysis bullosa (EB) – a disorder that makes the skin fragile and prone to blistering – had its roots in the expression of the gene COL7A1 in several types of prenatal skin cells.
Researchers were again able to compare gene expression in prenatal skin with their stem cell-derived lab-grown skin models and found strong similarities, noting that while these diseases often stem from defects in skin structure, they are frequently worsened by immune system involvement. [6]
The importance of stem cells and cord blood banking
As this new research demonstrates, stem cells play a pivotal role in not only helping researchers to better understand the formation of vital organs, like skin, but also in helping to facilitate potential future therapies.
By being able to compare cells from both prenatal and adult skin with artificial lab-grown skin using stem cells, researchers were able to identify the hitherto unknown significance of immune cells in skin formation and accurately map the genetic instructions involved in growing skin.
In their paper published in Nature, The Human Cell Atlas team have achieved something remarkable: essentially providing a set of instructions for creating human skin.
Their research is being heralded as groundbreaking and for good reason. Their findings will help to contribute to the development of a range of therapies for genetic skin conditions, treatments for wounds and burns, and remedies that could help to rejuvenate skin.
While the stem cells utilised in this trial were from embryonic stem cells and induced pluripotent stem cells, the stem cells found in umbilical cord tissue have similarly huge potential in regenerative medicine.
In fact, and as we’ve shown previously, trials utilising mesenchymal stem cells – the same type as found in umbilical cord tissue – are already underway that could aid in the treatment of both hair loss and skin conditions like atopic dermatitis. [7] [8]
What’s clear is that stem cells are pivotal in both cutting edge research and the development of future regenerative therapies.
Unfortunately, the umbilical cord and placenta – both rich sources of stem cells – are routinely thrown away after birth. By saving these powerful stem cells for your baby, you could give them access to future therapies that are currently being developed using stem cell-based research as in this study.
To find out more about saving stem cells for your baby, or the baby of someone you know who’s expecting, fill out the form below to download your free Welcome Pack.
References
[1] Ghosh, P. (2024, October 16). New skin research could help slow signs of ageing. BBC News. https://www.bbc.co.uk/news/articles/c756q166gd9o
[2] Gopee, N.H., Winheim, E., Olabi, B. et al. A prenatal skin atlas reveals immune regulation of human skin morphogenesis. Nature (2024). https://doi.org/10.1038/s41586-024-08002-x
[3] Lee J, Rabbani CC, Gao H, Steinhart MR, Woodruff BM, Pflum ZE, Kim A, Heller S, Liu Y, Shipchandler TZ, Koehler KR. Hair-bearing human skin generated entirely from pluripotent stem cells. Nature. 2020 Jun;582(7812):399-404. doi: 10.1038/s41586-020-2352-3. Epub 2020 Jun 3. PMID: 32494013; PMCID: PMC7593871.
[4] Martisova A, Sommerova L, Krejci A, Selingerova I, Kolarova T, Zavadil Kokas F, Holanek M, Podhorec J, Kazda T, Hrstka R. Identification of AGR2 Gene-Specific Expression Patterns Associated with Epithelial-Mesenchymal Transition. Int J Mol Sci. 2022 Sep 16;23(18):10845. doi: 10.3390/ijms231810845. PMID: 36142758; PMCID: PMC9504245.
[5] Gopee, N.H., Winheim, E., Olabi, B. et al. A prenatal skin atlas reveals immune regulation of human skin morphogenesis. Nature (2024). https://doi.org/10.1038/s41586-024-08002-x
[6] Huitema L, Phillips T, Alexeev V, Igoucheva O. Immunological mechanisms underlying progression of chronic wounds in recessive dystrophic epidermolysis bullosa. Exp Dermatol. 2021 Dec;30(12):1724-1733. doi: 10.1111/exd.14411. Epub 2021 Jun 27. PMID: 34142388; PMCID: PMC9290674.
[7] (2024, January 10). Stem Cells Could Be The Future of Hair Regrowth. Cells4Life. https://cells4life.com/2024/01/stem-cells-could-be-the-future-of-hair-regrowth/
[8] (2024, July 11). Promising Results of Stem Cell Eczema Treatment. Cells4Life. https://cells4life.com/2024/07/promising-results-of-stem-cell-eczema-treatment/
Last month researchers at The Parent’s Guide to Cord Blood Foundation compiled a report about how perinatal stem cells were being employed in clinical trials from 2019 through to the end of 2023. [1]
Perinatal stem cells are those which are collected in and around the perinatal period: the period immediately before and after birth.
These include stem cells from cord blood, cord tissue, the placenta and amnion.
In this blog, we’ll summarise some of their key findings and discuss what they mean in deciding to store stem cells for your baby.
Increase in the number of perinatal stem cell trials, despite COVID-19
In their report, researchers led by Dr Frances Verter point out how clinical trials using umbilical cord mesenchymal stem cells in particular reached a peak in 2020 and 2021, the result of accelerated research to help combat the COVID-19 pandemic.
They estimate that during the pandemic (2020-2022), nearly 41% of all advanced cellular therapy trials for COVID-19 relied on perinatal stem cells.
While the number of trials declined by almost half in the years that followed – to be expected, considering the impact of the pandemic on trial numbers – the researchers found that during the two years since their last report in 2021, the cumulative number of trials for advanced cellular therapies using perinatal stem cells increased by 17%.
This shows that the number of clinical trials using perinatal stem cells has not only returned to pre pandemic levels, but has actually increased, demonstrating a sustained interest in the clinical and therapeutic application of perinatal stem cells.
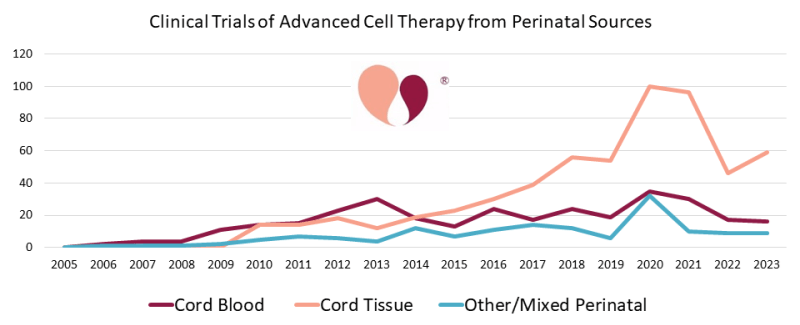
(graph courtesy of The Parents Guide to Cord Blood Foundation, https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells)
Trials for stem cells derived from placenta and amnion
Dr Verter and her team also point out that there are increasingly prominent roles for perinatal stem cells derived from a variety of sources beyond cord blood and cord tissue, namely: placenta and amnion.
Of the 402 clinical trials focusing on the use of mesenchymal stem cells derived or expanded from perinatal tissues, 9% utilised either placenta, amniotic membrane, or a mixture of a number of different perinatal stem cell sources. For reference, only 4% of trials derived MSCs from cord blood.
These numbers suggest that the placenta and amnion are becoming increasingly pivotal to the development of advanced cellular therapies using perinatal sources of stem cells, with the majority of these MSC trials focusing on COVID-19, neurological conditions, orthopaedic conditions and auto-immune disorders.
Cord tissue trials outpace cord blood trials
Since their last report on the cumulative number of trials through to the end of 2021, Dr Verter and her team found that in the years since, through to the end of 2023, there were 117 new trials utilising cord tissue and 40 new trials utilising cord blood. [2]
A key source of mesenchymal stem cells – which have the ability to differentiate into other specialised cell types such as muscle, nerve, and cartilage cells – cord tissue has once again shown itself to be at the forefront of trials utilising perinatal stem cells.
Of the 402 perinatal stem cell trials using MSCs, 87% of these utilised MSCs derived from cord tissue alone.
Considering that during the period from 2019-2023, over 75% of all perinatal stem cell trials were focused on the application of mesenchymal stem cells, cord tissue continues to be a vital source of the kind of stem cells that are driving current therapeutic interest in the application of stem cells from perinatal tissues.
Wide array of medical uses for perinatal mesenchymal stem cells
Another significant finding in this report is the sheer array of diagnosis categories that perinatal mesenchymal stem cells are being trialled for.
While around 45% of trials using perinatal mesenchymal stem cells focused on how they might be applied to treat COVID-19 and other respiratory illnesses, as well as neurological and orthopaedic conditions, another 46% of the total number of perinatal mesenchymal stem cell trials were divided across a wide range of medical diagnoses.
These medical diagnoses spanned trials for auto-immune disorders, the treatment of different forms of wounds, liver conditions, metabolic and genetic conditions (such as Krabbe disease and Hurler’s syndrome), cancers and blood cancers, and cardio-vascular conditions.
These figures suggest not only an increase in the number of perinatal mesenchymal stem cell trials, but also a broad spectrum of possible treatment applications, making them invaluable in the development of future advanced cellular therapies.
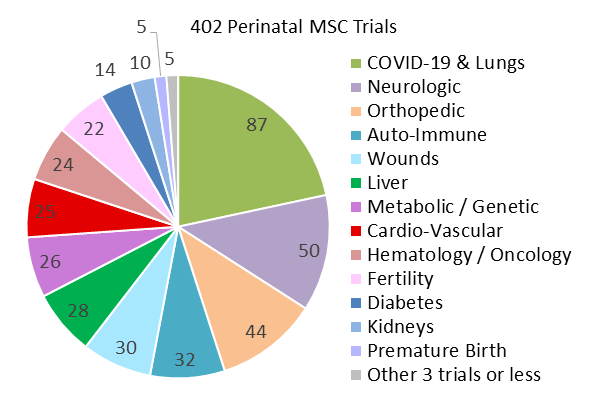
(graph courtesy of The Parents Guide to Cord Blood Foundation, https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells)
What does this mean for cord blood banking?
If you’re considering storing stem cells for your baby, the findings of this report are encouraging.
The sustained growth in clinical trials using perinatal stem cells, even beyond the pandemic, highlights the continued and expanding interest in their therapeutic potential.
Cord tissue, in particular, stands out as a critical source of mesenchymal stem cells, which are increasingly being used in a wide range of medical applications, from COVID-19 and neurological conditions to auto-immune disorders and orthopaedic treatments.
The growing use of placental and amniotic stem cells further emphasises the value of preserving these additional perinatal tissues, providing a great chance to maximise your baby’s ability to access future treatments.
With ongoing advancements in cellular therapies and the broad spectrum of diseases being targeted, banking stem cells from your baby’s umbilical cord and placenta could offer valuable opportunities for future medical treatments that go beyond what is available today.
Your baby’s stem cells may play a crucial role in the next generation of medical breakthroughs.
If you’re interested in storing stem cells for your baby, fill out the form below to request a free Welcome Pack. It contains information that will help to shed light on the collection process, our storage services, and the future potential offered by umbilical cord stem cells.
References
[1] Verter, F., Bersenev, A., & Couto, P. S. (2024, September 10). 2024 Update: How Many Clinical Trials Employ Perinatal Sources of Stem Cells? Parents Guide to Cord Blood Foundation. https://parentsguidecordblood.org/en/news/2024-update-how-many-clinical-trials-employ-perinatal-sources-stem-cells
[2] Verter, F. (2022, September 15). 2022 Update: How many clinical trials use cord blood or cord tissue? Parents Guide to Cord Blood Foundation. https://parentsguidecordblood.org/en/news/2022-update-how-many-clinical-trials-use-cord-blood-or-cord-tissue
04/12/2024 BlogStem Cell NewsStem Cell Therapies
Advancements in stem cell research are transforming how we approach some of the most critical health conditions.
One particularly exciting area is the use of umbilical cord stem cells in treating acute liver failure (ALF).
ALF is a life-threatening condition with limited treatment options, but new research suggests that umbilical cord-derived mesenchymal stem cells (UC-MSCs) could offer a promising solution.
What is Acute Liver Failure (ALF)?
Acute liver failure is a rare, though severe, condition comprising a rapid decline in liver function that can lead to severe health complications and even death if not treated promptly.
In the UK there are around 400 emergency admissions for ALF per year. Mortality rates for ALF are considerable: 60-90%. [1]
ALF is typically caused by viral infections, drug toxicity, or autoimmune diseases.
Most admissions in the UK were for paracetamol overdoses.
Current treatment options are limited to liver transplants or supportive care—both of which come with significant obstacles, including lack of available organs and financial expense. [2]
As a result, there is a growing need to explore alternative therapies, and stem cells from the umbilical cord show huge potential for application in treatment.
How could umbilical cord stem cells help?
The umbilical cord is a rich source of mesenchymal stem cells. These are cells that have the ability to differentiate into other specialised cell types in the body, as well as having immunomodulatory properties and the ability to secrete growth factors. [3]
While MSCs can be derived from various sources, including bone marrow and adipose tissue, numerous studies have shown that the use of mesenchymal stem cells derived from the umbilical cord in the treatment of ALF is associated with lower mortality rates and improved liver function. [4] [5]
It’s also been suggested that UC-MSCs are better positioned to both differentiate into hepatocyte-like cells (i-Heps) and promote the proliferation of hepatocyte cells within the liver. [6]
Hepatocyte cells are responsible for various processes within the liver, and cause inflammation when they become damaged, a contributing factor to ALF. [7]
The ability to either replace damaged hepatocyte cells or promote their proliferation using UC-MSCs could be hugely important in mitigating acute liver failure.
What’s the latest research into using umbilical cord stem cells for ALF?
A new clinical trial is currently underway exploring the use of mesenchymal stem cells derived from the umbilical cord (UC-MSCs) as a treatment option for ALF.
The trial, which is scheduled to conclude in 2028, will assess the safety and efficacy of UC-MSCs in cases of acute-on-chronic liver failure wherein patients experience sudden organ failure as a result of an underlying chronic liver disease.
A multi-centred, double blind and randomised placebo controlled trial, the new study will seek to validate previously promising findings about the use of MSCs in acute liver failure treatment.
Participants will be split into a control group and a treatment group, with those in the treatment group receiving either 3 or 5 intravenous infusions of mesenchymal stem cells depending on whether they are members of the short or prolonged treatment group.
Follow-ups will occur weekly up to 5 weeks and then at 8, 12, 24, and 53 weeks.
The trial will also seek to definitively determine whether umbilical cord-derived mesenchymal stem cells are more effective than other sources of MSCs in the treatment of acute liver failure. [8]
Cord blood banking and ALF treatment
This study is just one of many showing the therapeutic potential of umbilical cord stem cells, not just for ALF, but for a variety of conditions.
There are currently hundreds of clinical trials exploring how umbilical cord stem cells could help in the treatment of conditions ranging from cancer to stroke, heart disease to Parkinson’s disease.
For patients with acute liver failure, UC-MSC-based therapy could one day become a life-saving alternative to liver transplants.
As this research progresses, cord blood banking becomes even more valuable as it means having your own perfectly matched stem cells available for use in future therapies, eliminating the risk of rejection.
If you or someone you know is expecting, download our free Welcome Pack below to find out more about saving baby’s stem cells. It could be the best decision you ever make for their health.
References
[1] Kerslake, D. A. (2024, August 5). Acute Liver Failure. RCEM Learning. https://www.rcemlearning.co.uk/reference/acute-liver-failure/#1567604193379-1229443a-872e
[2] Wang, Y. H., & Chen, E. Q. (2023). Mesenchymal Stem Cell Therapy in Acute Liver Failure. Gut and liver, 17(5), 674–683. https://doi.org/10.5009/gnl220417
[3] Hu, C., Wu, Z., & Li, L. (2020). Mesenchymal stromal cells promote liver regeneration through regulation of immune cells. International journal of biological sciences, 16(5), 893–903. https://doi.org/10.7150/ijbs.39725
[4] Xu, W. X., He, H. L., Pan, S. W., Chen, Y. L., Zhang, M. L., Zhu, S., Gao, Z. L., Peng, L., & Li, J. G. (2019). Combination Treatments of Plasma Exchange and Umbilical Cord-Derived Mesenchymal Stem Cell Transplantation for Patients with Hepatitis B Virus-Related Acute-on-Chronic Liver Failure: A Clinical Trial in China. Stem cells international, 2019, 4130757. https://doi.org/10.1155/2019/4130757
[5] Shi, M., Zhang, Z., Xu, R., Lin, H., Fu, J., Zou, Z., Zhang, A., Shi, J., Chen, L., Lv, S., He, W., Geng, H., Jin, L., Liu, Z., & Wang, F. S. (2012). Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem cells translational medicine, 1(10), 725–731. https://doi.org/10.5966/sctm.2012-0034
[6] Zhou, R., Li, Z., He, C., Li, R., Xia, H., Li, C., Xiao, J., & Chen, Z. Y. (2014). Human umbilical cord mesenchymal stem cells and derived hepatocyte-like cells exhibit similar therapeutic effects on an acute liver failure mouse model. PloS one, 9(8), e104392. https://doi.org/10.1371/journal.pone.0104392
[7] Gong, J., Tu, W., Liu, J., & Tian, D. (2023). Hepatocytes: A key role in liver inflammation. Frontiers in immunology, 13, 1083780. https://doi.org/10.3389/fimmu.2022.1083780
[8] Wang, Y., Li, M., Yang, T., Xie, Y., Wang, F. S., Hu, J., & Shi, M. (2024). Human umbilical cord mesenchymal stem cell transplantation for the treatment of acute-on-chronic liver failure: protocol for a multicentre random double-blind placebo-controlled trial. BMJ open, 14(6), e084237. https://doi.org/10.1136/bmjopen-2024-084237
A new clinical trial investigating the use of umbilical cord stem cells to treat chronic heart failure is currently underway.
The Phase II trial, which is the first of its kind in the U.S., is being carried out by researchers at the University of Louisville. It’s also the first time intravenous (IV) delivery will be trialled for the delivery of cell therapy for heart failure. [1]
It’s hoped that this pioneering approach could change the way that heart failure patients are treated.
What is heart failure?
Heart failure arises when the heart can’t pump blood around the body properly. This results in the body being unable to receive the oxygen it needs to function normally.
Heart failure can arise from various causes, with some of the most common being:
-
Cardiomyopathy: A condition where the heart’s muscular wall thickens, making it difficult for the heart to effectively pump blood throughout the body.
-
Heart Attack: A heart attack can cause lasting damage to the heart, impairing its ability to circulate blood efficiently.
-
High Blood Pressure: Chronic high blood pressure puts strain on the heart, gradually reducing its pumping efficiency.
-
Abnormal Heart Rhythms: An irregular, too slow, or too fast heartbeat can disrupt the heart’s normal pumping function. [2]
It’s estimated that heart failure affects more than a million people in the U.K. and at least 64 million people worldwide. [3]
Heart failure usually gets worse over time. However, while there is no cure, there are steps that can be taken to treat and manage symptoms, including surgery, having a pacemaker fitted, medication, and lifestyle changes. [4]
What is the new stem cell trial for heart disease?
The trial, which has been dubbed ‘CATO’, will enrol 60 participants across 3 locations, all of whom would have suffered from ischemic cardiomyopathy – heart failure arising from the damage caused by heart attack.
Conducted on a randomised, double blind and placebo controlled basis to ensure rigorous scientific standards, participants will be split into three groups: a control group, a single dose group and a multiple dose group.
All participants will receive four infusions delivered via IV over the course of 2 months.
The control group will receive four doses of placebo, the single dose group will receive one dose of umbilical cord-derived mesenchymal stem cells (UC-MSCs) and three doses of placebo, and the multiple dose group will receive four doses of UC-MSCs.
The first trial to test the delivery of cell therapy for heart failure in multiple doses, CATO will not only investigate the effectiveness of using UC-MSCs for treating heart failure, but also the effectiveness of their delivery in multiple infusions.
Participants will be monitored at intervals of 2 hours, 1 week, and 2 months after each infusion and then followed for 6 months after all four infusions to monitor the safety and efficacy of the therapy. [5]
Why are umbilical cord stem cells being used in the heart failure trial?
Previous studies have shown that mesenchymal stem cells derived from the umbilical cord have abilities that make them ideal in the treatment of cardiovascular diseases.
These include the ability to differentiate into cardiovascular progenitor cells, to modulate immune responses, and promote growth factors. [6] [7]
These cells, harvested from donated umbilical cords, have shown promise in treating a range of conditions, including ulcerative colitis, Crohn’s disease, and even COVID-19. [8] [9] [10]
Now, for the first time in the United States, they are being tested in heart failure patients.
UC-MSCs offer several advantages in this area over other types of stem cells.
Most notably, UC-MSCs can be isolated, stored frozen and then expanded into large quantities, making them readily available “off the shelf” when needed.
This reduces both the cost and the time required to initiate treatment, making it more accessible to a broader range of patients. [11]
Researchers leading the trial hope that umbilical cord-derived mesenchymal stem cells will provide a new and much needed therapeutic alternative in the treatment of heart failure.
Should I save my baby’s umbilical cord stem cells?
This trial demonstrates the growing interest and potential of umbilical cord stem cells to combat conditions, like heart failure, that are currently incurable.
If you have a history of heart disease in your family, it’s probably worth saving the stem cells from your baby’s umbilical cord.
While the stem cells used in this trial will be sourced from donated umbilical cords, privately storing the stem cells from your baby’s umbilical cord rules out the risk of rejection by ensuring that they always have access to stem cells from their own perfect match: themselves.
It also gives them the best chance of accessing future stem cell therapies currently being developed in clinical trials not just for heart failure but also for diseases and conditions like cancer, stroke, and Parkinson’s disease.
If you or a family member are expecting and want to know more about private stem cell storage, fill out the form below to receive your free Welcome Pack.
References
[1] UofL News (2024, August 6). UofL cardiologist leading clinical trial for high potential new therapy for heart failure. University of Louisville School of Medicine. https://louisville.edu/medicine/news/uofl-cardiologist-leading-clinical-trial-for-high-potential-new-therapy-for-heart-failure
[2] Heart failure. British Heart Foundation. https://www.bhf.org.uk/informationsupport/conditions/heart-failure?gad_source=1&gclid=Cj0KCQjww5u2BhDeARIsALBuLnP2GAM0j5TBp0pX-OL9l3Vgzt8yZWBcKKk8j5T0m_JI8pHKPqZKiY8aAi02EALw_wcB&gclsrc=aw.ds
[3] Nicola Luigi Bragazzi, Wen Zhong, Jingxian Shu, Arsalan Abu Much, Dor Lotan, Avishay Grupper, Arwa Younis, Haijiang Dai, (2021) Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017, European Journal of Preventive Cardiology, Volume 28, Issue 15, December 2021, Pages 1682–1690, https://doi.org/10.1093/eurjpc/zwaa147
[4] (2022, May 19). Overview: Heart failure. NHS. https://www.nhs.uk/conditions/heart-failure/
[5] (2024, June 13). Single or Repeated Intravenous Administration of umbiliCAl Cord Mesenchymal sTrOmal Cells in Ischemic Cardiomyopathy (CATO). ClinicalTrials.gov. https://clinicaltrials.gov/study/NCT06145035
[6] Abouzid, M. R., Ali, K., Kamel, I., Esteghamati, S., Saleh, A., & Ghanim, M. (2023). The Safety and Efficacy of Human Umbilical Cord-Derived Mesenchymal Stem Cells in Patients With Heart Failure and Myocardial Infarction: A Meta-Analysis of Clinical Trials. Cureus, 15(11), e49645. https://doi.org/10.7759/cureus.49645
[7] Bartolucci, J., Verdugo, F. J., González, P. L., Larrea, R. E., Abarzua, E., Goset, C., Rojo, P., Palma, I., Lamich, R., Pedreros, P. A., Valdivia, G., Lopez, V. M., Nazzal, C., Alcayaga-Miranda, F., Cuenca, J., Brobeck, M. J., Patel, A. N., Figueroa, F. E., & Khoury, M. (2017). Safety and Efficacy of the Intravenous Infusion of Umbilical Cord Mesenchymal Stem Cells in Patients With Heart Failure: A Phase 1/2 Randomized Controlled Trial (RIMECARD Trial [Randomized Clinical Trial of Intravenous Infusion Umbilical Cord Mesenchymal Stem Cells on Cardiopathy]). Circulation research, 121(10), 1192–1204. https://doi.org/10.1161/CIRCRESAHA.117.310712
[8] Lin, Y., Lin, L., Wang, Q., Jin, Y., Zhang, Y., Cao, Y. and Zheng, C. (2015), Transplantation of human umbilical mesenchymal stem cells attenuates dextran sulfate sodium-induced colitis in mice. Clin Exp Pharmacol Physiol, 42: 76-86. https://doi.org/10.1111/1440-1681.12321
[9] Zhang, J., Lv, S., Liu, X., Song, B., & Shi, L. (2018). Umbilical Cord Mesenchymal Stem Cell Treatment for Crohn’s Disease: A Randomized Controlled Clinical Trial. Gut and liver, 12(1), 73–78. https://doi.org/10.5009/gnl17035
[10] Guo, B. C., Wu, K. H., Chen, C. Y., Lin, W. Y., Chang, Y. J., Lee, T. A., Lin, M. J., & Wu, H. P. (2023). Mesenchymal Stem Cells in the Treatment of COVID-19. International journal of molecular sciences, 24(19), 14800. https://doi.org/10.3390/ijms241914800
[11] UofL News (2024, August 6). UofL cardiologist leading clinical trial for high potential new therapy for heart failure. University of Louisville School of Medicine. https://louisville.edu/medicine/news/uofl-cardiologist-leading-clinical-trial-for-high-potential-new-therapy-for-heart-failure
24/10/2024 BlogNewsStem Cell NewsStem Cell Therapies
Last week it was announced that a new gene editing stem cell therapy for beta thalassemia would start to be made available on the NHS.
The therapy, called Casgevy, is developed by Vertex Pharmaceuticals and CRISPR Therapeutics and received approval from the UK regulator in November of last year. You can read about that announcement here.
It’s estimated that there are approximately 460 patients aged 12 or older with transfusion dependent beta thalassemia in England who are currently eligible for the treatment.
According to the NHS, the therapy will be offered across seven specialist centres and manufactured in the UK. [1]
What is beta thalassemia?
Beta thalassemia is an inherited blood disorder which affects the production of haemoglobin, a protein in red blood cells used to carry oxygen around the body.
Those affected by beta thalassemia produce little to no haemoglobin and as a result require frequent blood transfusions to supply red blood cells that can carry oxygen to tissues in the body.
Symptoms of beta thalassemia are associated with anaemia and range from mild – fatigue, weakness, headaches – to severe: heart palpitations, abdominal swelling, and jaundice.
Beta thalassemia has a debilitating impact on sufferers’ quality of life and it can also dramatically reduce life expectancy. [2]
What is Casgevy and how does it work?
The new therapy utilises a combination of the patient’s own stem cells and gene editing technology to reprogramme cells so that they produce healthy red blood cells.
Once the stem cells are harvested from the patient’s bone marrow they are then sent to a lab to undergo modification using the gene-editing tool CRISPR.
CRISPR effectively works like a pair of highly-targeted scissors, seeking out a specific section of DNA and editing a specific gene within it. In this instance, CRISPR targets the gene BCL11A.
During foetal development the body produces a unique form of haemoglobin in order to extract oxygen from the mother’s bloodstream. Once we’re born, BCL11A is responsible for silencing the production of foetal haemoglobin so that beta, or adult, haemoglobin can begin to be produced.
By targeting the BCL11A gene, the CRISPR tool is able to reverse the silencing process and re-encourage the production of foetal haemoglobin which, crucially, is left unaffected by beta thalassemia.
Once the stem cells have been edited to turn off BCL11A, they are then returned to patients via infusion and take residence in the bone marrow. The new, edited stem cells then begin to produce healthy red blood cells. [3]
In clinical trials, the new therapy removed the need for blood transfusions for at least a year in 39 of the 42 beta thalassemia sufferers treated. [4]
What’s next for the new therapy?
While the cost to the NHS of the new therapy is hefty – an estimated £1.6 million per patient – the treatment is being heralded as a cure, with the added benefit of eradicating the need for frequent blood transfusions, thereby reducing strain on healthcare services and improving patients’ quality of life outcomes.
With the new therapy expected to be rolled out in the coming weeks, attention now turns to whether the Casgevy treatment for sickle cell anaemia – another blood disorder affecting haemoglobin – will also be offered on the NHS, after its approval in November last year. [5]
What does this mean if I want to store my baby’s stem cells?
If it’s likely your baby could have beta thalassemia, it’s probably worth considering banking their umbilical cord blood.
Umbilical cord blood is rich in haematopoietic stem cells which are already being used in over 80 approved treatments, including for blood disorders.
Giving your baby the gift of stem cell storage may mean that they’ll one day be able to use their cord blood stem cells for the Casgevy therapy instead of the more intrusively procured bone marrow stem cells.
While not currently an approved version of the procedure, using the stem cells from banked umbilical cord blood rather than bone marrow could make for a less invasive procedure overall for your child, should they ever need it.
To find out more about how banking your baby’s stem cells could give them access to future medical advancements, request your free Welcome Pack below.
References
[1] (2024, August 8). Gene-editing therapy that could cure blood disorder thalassaemia for NHS patients. NHS England. https://www.england.nhs.uk/2024/08/gene-editing-therapy-that-could-cure-blood-disorder-thalassaemia-for-nhs-patients/#:~:text=The%20one%2Doff%20gene%20therapy,a%20severe%20form%20of%20thalassaemia.
[2] (2022, July 20). Beta Thalassemia. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23574-beta-thalassemia
[3] Gallagher, J. (2024, August 8). First gene-editing therapy may cure blood disorder. BBC News. https://www.bbc.co.uk/news/articles/c4gzldll44lo
[4] (2024, June 14). Vertex Presents Positive Long-Term Data On CASGEVY™ (exagamglogene autotemcel) at the 2024 Annual European Hematology Association (EHA) Congress. Vertex. https://news.vrtx.com/news-releases/news-release-details/vertex-presents-positive-long-term-data-casgevytm-exagamglogene
[5] (2024, August 8). World’s first gene editing therapy for blood disorder to be available to hundreds of patients in England. National Institute for Health and Care Excellence. https://www.nice.org.uk/news/articles/worlds-first-gene-editing-therapy-for-blood-disorder-to-be-available-to-hundreds-of-patients-in-england
24/10/2024 BlogNewsStem Cell NewsStem Cell Therapies
















